Healthcare Associated Infections (HAIs) acquired in a hospital or healthcare service unit, appear 48 hours or more after hospital admission, or within 30 days after discharge following patient care1. Contaminated surfaces within a hospital environment play a crucial role in the transmission of HAIs and are a result of numerous pathogenic species, including methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus species, Clostridioides difficile, Acinetobacter species and even viruses such as Norovirus2. Infection with any one of these pathogenic species can lead to a wide variety of symptoms, including fever, coughs, nausea, vomiting, headaches, or shortness of breath.
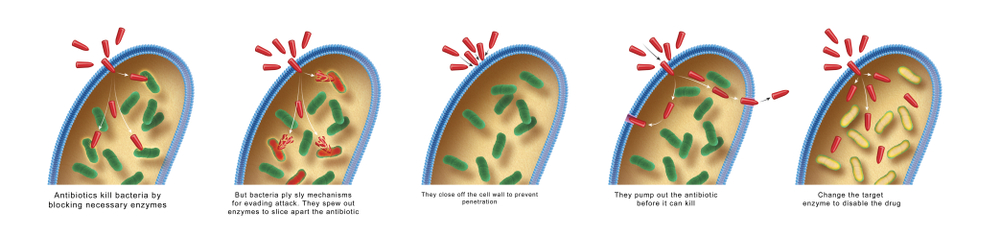
Due to the immunocompromised condition of many hospital patients, HAIs can spread rapidly via person-to-person contact because of unclean hands, medical instruments, respiratory machines, and other hospital tools. HAI cases also increase when there has been excessive and improper use of antibiotics, which can lead to bacteria which are resistant to multiple antibiotic treatments3.
Biofilms can also grow inside wounds
It is the growth of such multi-resistant microorganisms, within a biofilm, that has posed the greatest challenge in treating HAIs, owing to the association of biofilms with increased resistance to antimicrobial therapies4. A biofilm is a gathering of surface-associated microbial cells which attach to one another. These microbial cells can produce extracellular proteins which allow for attachment to surfaces while producing a matrix which forms a protective barrier surrounding the cells5. Biofilms are the leading cause of HAIs and can grow on medical devices, such as heart valves and pacemakers, as well as on any surface within a patient’s treatment room, even sprouting tiny legs which they can use to walk across surfaces6. Biofilms can also grow inside wounds.
HAIs can occur in both adult and pediatric patients. The most common types of HAIs seen in children are bloodstream infections, pneumonia, urinary tract infections, skin, and surgical site infections7. In Europe, incidence rates of HAIs in General Pediatric wards are 1%, while infection rates of up to 23.6% are observed in Pediatric Intensive care units (ICUs)8. From 2011-2012, the European Centre for disease prevention and control (ECDC) held the first Europe-wide prevalence study of HCAIs in acute care hospitals. Data from over 17,273 children and adolescents showed a HAIs prevalence rate of 15.5% in pediatric ICUs and 10.7% in neonatal ICUs9.
“When we look back at our data from the studies, we’ve known for long-time floors are a reservoir for a lot of different bacteria. Primarily, in this case, that’s what we’re looking at, and how difficult it is for any facility to really keep floors clean, especially in high traffic areas”
Research from Levine et al., 2022, revealed that the floors of hematology/oncology (HO) units in pediatric wards were contaminated with Clostridioides difficile (25–29% of floors swabbed) and MRSA (26.9-42.3% of floors swabbed), two of the most common HAI pathogens10. This recent 10-month study was carried out by medical specialists at the University of Tennessee and was showcased at the APIC (Association for Professionals in Infection Control and Epidemiology) 2022 Annual Conference. As stated by Levine, “When we look back at our data from the studies, we’ve known for long-time floors are a reservoir for a lot of different bacteria. Primarily, in this case, that’s what we’re looking at, and how difficult it is for any facility to really keep floors clean, especially in high traffic areas”.

A second study was carried out to determine the presence of Staphylococci in neonatal ICUs.
Results indicated that the floors by the sinks of these neonatal ICUs were contaminated by MRSA in 76.2% of samples taken, and Staphylococcus aureus in 87.3% of samples taken. MRSA was also present at the foot of the neonatal bed (5.7%) and on the suction tips (25.7%)11.
These studies discovered the flaws in hygiene and bacterial prevention in hospitals. Ideally, no one should catch an infection while receiving health care, yet these infections can spread rapidly and are a common occurrence which affects hundreds of millions of people each year. These research efforts highlight the need for new and efficient cleaning products, as well as infection prevention methods, to reduce the risk of MRSA and Clostridioides difficile on floors, and surfaces alike. With immunocompromised children at risk, additional measures are necessary to ensure cleaning strategies are effective for these at-risk patients.
At Medentech, we manufacture a range of high-level broad-spectrum NaDCC disinfectant tablets that are used in hospitals globally to kill harmful viral and bacterial pathogens on surfaces. Our products Klorsept and Klorkleen 2, are included in the EPA N list of products that meet EPA’s criteria for use against SARS-CoV-2 and are approved by EPA as fast, effective against surface biofilm and C. diff Spores. For more information on the sustained residual efficacy of our products on surface biofilm and C.diff click here
References
1 Revelas A. Healthcare - associated infections: A public health problem. Niger Med J. 2012 Apr;53(2):59-64. doi: 10.4103/0300-1652.103543. PMID: 23271847; PMCID: PMC3530249. 2 Weber, David J.a,b; Anderson, Deverickc; Rutala, William A.a,b The role of the surface environment in healthcare-associated infections, Current Opinion in Infectious Diseases: August 2013 - Volume 26 - Issue 4 - p 338-344 doi: 10.1097/QCO.0b013e3283630f04 3 Hospital-Acquired Infection: Definition and Patient Education (healthline.com) 4 Percival SL, Suleman L, Vuotto C, Donelli G. Healthcare-associated infections, medical devices and biofilms: risk, tolerance and control. J Med Microbiol. 2015 Apr;64(Pt 4):323-334. doi: 10.1099/jmm.0.000032. Epub 2015 Feb 10. PMID: 25670813. 5 Rodney M. Donlan, Biofilm Formation: A Clinically Relevant Microbiological Process, Clinical Infectious Diseases, Volume 33, Issue 8, 15 October 2001, Pages 1387–1392, https://doi.org/10.1086/322972 6 https://www.statnews.com/2016/06/28/biofilms-bacteria-research/ 7 Becerra MR, Tantalean JA, Suarez VJ, Alvarado MC, Candela JL, Urcia FC. Epidemiologic surveillance of nosocomial infections in a Pediatric Intensive Care Unit of a developing country. BMC Pediatr. 2010;10:66. doi: 10.1186/1471-2431-10-66. 8 Raymond J, Aujard Y, Bekassi A, the European Study Group: Nosocomial infections in pediatric patients: a European, multicenter prospective study. Infect Control Hosp Epidemiol. 2000, 21: 260-263. 10.1086/501755. 9 Zingg W, Hopkins S, Gayet-Ageron A, Holmes A, Sharland M, Suetens C; ECDC PPS study group. Health-care-associated infections in neonates, children, and adolescents: an analysis of paediatric data from the European Centre for Disease Prevention and Control point-prevalence survey. Lancet Infect Dis. 2017 Apr;17(4):381-389. doi: 10.1016/S1473-3099(16)30517-5. Epub 2017 Jan 13. PMID: 28089444. 10 David Levine, Henry G. Spratt, Jennifer A. Keates-Baleeiro, Lindsey Brunton, William Gaylord. Bacterial Contamination of Floors in a Hematology/Oncology Unit in a Children's Hospital, American Journal of Infection Control, Volume 50, Issue 7, Supplement, 2022, Page S13. ISSN 0196-6553.https://doi.org/10.1016/j.ajic.2022.03.080. 11 Henry G. Spratt, David Levine, Anuj Sinha, Daniel See. Surveillance of Staphylococci Presence in and Around Neonate Isolette Beds in a Neonatal Intensive Care Unit of a Children's Hospital, American Journal of Infection Control, Volume 50, Issue 7, Supplement, 2022, Page S15. ISSN 0196-6553. https://doi.org/10.1016/j.ajic.2022.03.085.